Find us in your favorite podcast app:
Spotify
SoundCloud
iTunes
Stitcher
Subscribe to the Ganjapreneur podcast on iTunes, Stitcher, SoundCloud or Google Play.
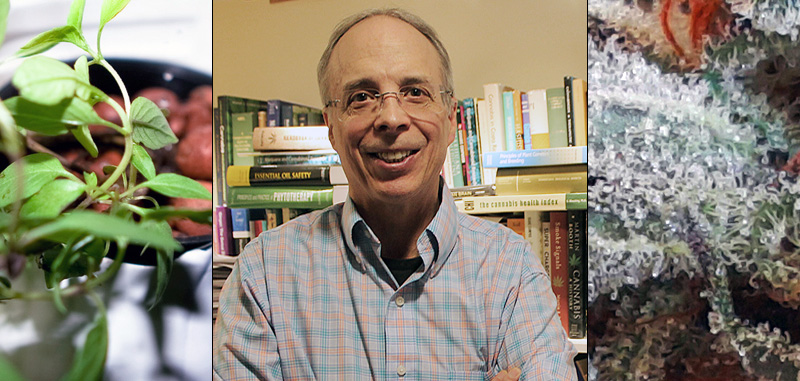
Our latest podcast interview features Dr. Ethan Russo, formerly Senior Medical Advisor to GW Pharmaceuticals, who participated in three clinical trials of the drug Sativex. Dr. Russo recently left GW Pharmaceuticals and can now speak publicly for the first time about his research: up until now, he could only be heard at expensive, exclusive conferences. He is now Medical Director at Phytecs, a company specializing in the production of cannabis-based treatments related to the endocannabinoid system. Everything that contemporary cannabis healers talk about in relation to cannabis as medicine is based on Dr. Russo’s published research, including the power of cannabis terpenes, the Entourage Effect, and Endocannabinoid Deficiency.
In this interview, our host Shango Los asks Dr. Russo about Endocannabinoid Deficiency (ECD) and the potential for it to be treated by cannabis. All human beings have an endocannabinoid system, which, according to Russo, regulates nearly every aspect of physiology. The Phytecs website states:
“The endocannabinoid system (ECS) is a homeostatic regulatory system that forms the cornerstone of a vast signaling network found in all vertebrates including humans. The ECS effectively ‘regulates regulation’ for physiological processes.”
Endocannabinoid Deficiency is just coming into general awareness now as a cause behind several conditions including Migraines, Fibromyalgia, Irritable Bowel Syndrome, Phantom Limb Pain, Infantile colic, Glaucoma, PTSD, Bipolar disease and others. If cannabis becomes accepted by the mainstream medical community as a treatment for ECD and its associated conditions, the implications for the pharmaceuticals market would be staggering to say the least. Listen to the podcast or read the transcript below to learn about the science behind ECD and how Dr. Russo believes cannabis can be used as a treatment!
Subscribe to the Ganjapreneur podcast on iTunes, Stitcher, SoundCloud or Google Play.
Listen on Soundcloud:
Read the Full Transcript:
Shango Los: Welcome to the Ganjapreneur.com podcast. My name is Shango Los and I will be your host today.
Ethan Russo, MD, is a board-certified neurologist, psychopharmacology researcher, and former Senior Medical Advisor to GW Pharmaceuticals. He served as study physician to GW Pharmaceuticals for three Phase III clinical trials of the cannabis drug Sativex.
He graduated from the University of Pennsylvania and the University of Massachusetts Medical School, before residencies in Pediatrics in Phoenix, Arizona and in Child and Adult Neurology at the University of Washington in Seattle. He was a clinical neurologist in Missoula, Montana for 20 years in a practice with a strong chronic pain component. In 1995, he pursued a 3-month sabbatical performing ethnobotanical research with indigenous people in Peru. He joined GW as a full-time consultant in 2003.
He is currently past president of the International Cannabinoid Research Society and is former chairman of the International Association for Cannabinoid Medicines. He is author of the Handbook of Psychotropic Herbs, co-editor of Cannabis and Cannabinoids: Pharmacology, Toxicology and Therapeutic Potential and author of The Last Sorcerer: Echoes of the Rainforest. He was founding editor of the Journal of Cannabis Therapeutics, selections of which were published as books; Cannabis Therapeutics in HIV/AIDS, Women and Cannabis: Medicine, Science and Sociology, and Cannabis: From Pariah to Prescription and so many more.
He is presently medical director at PHYTECS, an American company developing endocannabinoid-based medicines. Everything that contemporary cannabis cures talk about in relation to cannabis as medicine is based on Ethan’s published research; cannabis terpenes, their human powers and volatility, the entourage effect and whole plant medicine and endocannabinoid deficiency. Today he is here to speak with us about endocannabinoid deficiency. Welcome, Dr. Russo.
Ethan Russo: Thank you.
Shango Los: Dr. Russo, your research supports that each human has an underlying endocannabinoid tone that reflects the state of their body’s cannabinoid receptors and that a deficient amount of endocannabinoids can lead to all sorts of physical failures in the body. Would you explain to me what you mean by endocannabinoid tone and how it offers insights to the state of the body as a whole?
Ethan Russo: Sure. The endocannabinoid system is a system in the body that is one that promotes homeostasis, a balance in other functions. It consists of 3 components. There are cannabinoid receptors in the body where THC in cannabis binds, but the endocannabinoid system is a lot older than cannabis so cannabis is not there just to get as high. This doesn’t have the system originated rather these receptors are in the brain, one called CB1.
Cannabinoid 1 is the psychoactive receptor. This is where THC works, but it has many important functions in the brain, including regulation of pain, seizure threshold whether someone will be epileptic or not, whether they become nauseated. It regulates levels of neurotransmitters, chemical messengers in the brain. Additionally, there’s a CB2, another receptor that’s mainly thought of as being out in the body where it’s involved in again regulation of pain and inflammatory responses. The receptors are 1 component of the endocannabinoid system.
There are endogenous cannabinoids. These are natural chemicals in the body, anandamide and 2HE; their names are the best characterized ones. These resemble THC in their activity. A lot of what THC does is paralleled by the effects of these natural chemicals in the body that everyone has.
The third component of the endocannabinoid system is the enzymes that make the endocannabinoids and break them down. If there are too many receptors or too much endocannabinoid or there is a deficit in enzymatic activity, any of these things can throw the balance off in the system. Someone having decreased endocannabinoid count could come about because they have too few receptors or they too few endocannabinoids, but ultimately the body tries to keep these in balance so that the systems work at their best.
Shango Los: The endocannabinoid tone itself in your papers it sounds like that maybe a quantifiable or measurable thing. What exactly would you say the endocannabinoid tone is?
Ethan Russo: It would reflect the amount of endogenous cannabinoids in the body that would be one, but it would also be affected by the number of receptors that were active and that’s something that can be influxed. It can change upwards or downwards. Let me give an example.
If someone uses a great deal of cannabis daily, it will actually down regulate the receptor. In other words the body tries to prevent excesses of activity and it will do that by inactivating the receptor if there’s too much activity, so that could happen. There are also things that can up regulate the receptor, make it more active.
It is a function of all 3 and it’s not an easy thing to measure either. I’m sure that people wonder already they might have an endocannabinoid deficiency. Right now this isn’t accessible by any simple blood test. The amount of say anandamide, one of the endocannabinoids, in the blood can be measured but with great differently. It’s a research technique.
The material actually breaks down so rapidly that if someone’s blood sample is taken to test it. It’s got to be immediately put in a liquid nitrogen and send off to a specialty lab that does this work. Certainly, it’s not available at your friendly local hospital to test.
In actuality, the best way to test won’t be in the blood. Most of these conditions would be reflected in brain activity. A better way would be to test this rigorous spinal fluid that’s what you get when a spinal tap or lumbar puncture is done. Because that’s an invasive procedure, we don’t do that in this situation except as a research technique either.
Someday hopefully soon there might be a way to do imaging of the brain to assess the endocannabinoid activity that would be the best way hopefully without requiring any needle sticks or anything else that’s invasive. Right now for most people this is going to be what we call a diagnosis of exclusion meaning that if other things are not identified as the culprit it may be that this is going on. It will be what’s called the clinical diagnosis based on the pattern of the illness.
Shango Los: In the idea of the tone it sounds like if you have too many or too little on either side of the relationship either between the receptors or the cannabinoids themselves that is where the issue is. Does it not really matter if you have a smaller relationship, less receptors and less cannabinoids or more receptors and more cannabinoids that is in as much of the difference? The question is whether or not they are equal.
Ethan Russo: I think you’ve identified the issue. You can have too many receptors but not enough endocannabinoids. Really they need to be in balance. This brings to the fore an issue I should emphasize at this point. The whole function of the endocannabinoid system is what’s called as a homeostatic regulator. Let’s break that down.
Homeostasis is a balance in bodily function. The endocannabinoid system regulates how other aspects of physiology, how our body works. Let’s give a couple of examples. One of the main things the endocannabinoid system does in the brain is regulate the amount of neurotransmitters, their activity.
Neurotransmitters are chemical messengers in the brain that allow 1 nerve to talk to another. Let’s say for example that there’s too much glutamate activity. This is one of those neurotransmitters. It’s stimulatory, in other words 1 nerve communicating with the next increases its signal. That’s all well and good. It’s a necessary function but when it’s present in excess it will do 2 things that are potentially bad.
One is it produces neuropathic pain, nerve-based pain, a very severe kind of pain that’s associated with nerve problems out in the body or nerve damage in the brain, that’s one. Additionally, glutamate activity is excessive after head injury or strokes so much so that actually can kill brain cells. See, understand then that if there’s too much glutamate that the endocannabinoid system if it’s able to bring those levels down is a helpful thing in promoting health. If we look at systems beyond the brain, the digestion, hormonal systems, the skin, regulation of pain, whether or not somebody have a seizure, all of these are regulated by the endocannabinoid system.
Now the really surprising thing is this system has only been described for about 20 years, a little bit more. We wouldn’t know about it yet maybe if we didn’t know about cannabis, because it was through the study of THC and cannabis and other cannabinoids that this system was discovered. It likely would have taken another 1 or 2 decades to recognize it and its importance have it not been for this relationship.
Shango Los: If the cannabinoid receptors being out of balance causes impacts, it begs the question for patients at home who are self medicating with cannabis. Is it possible that they could intake too much of cannabinoid precursors or through like RSO or something and end up over flushing their brain with endocannabinoids and throwing themselves out of whack?
Ethan Russo: That’s certainly a risk. Most cannabis-based therapeutic requires very low doses, particularly of THC. The tincture in excessive intake is what’s called tolerance or down regulation. We mentioned a little while ago that if there’s too much activity the cannabinoid receptors will become less active. This is what happens when somebody uses so much THC that they become tolerant to it. What the consumer would notice is the amount of cannabis that previously would give them the effect they want saying feeling high no longer work that they needed a lot more in contrast.
When people are treating symptoms particularly those associated with what we call clinical endocannabinoid deficiency and that would be migraine, fibromyalgia and idiopathic bowel syndrome or spastic colon those 3 examples. What they seem to respond to in contrast are very low doses of a cannabis-based medicine and that could be low doses of THC or perhaps higher doses of cannabidiol, which tends to itself promote the function of anandamide, one of the endocannabinoids and help bring the systems into balance better.
Shango Los: 2 of the ailments they talked about in your research are both the bowel syndrome and migraine. As a migraine sufferer, I was very interested in r6eading the specific mechanics of how the endocannabinoid tone being out of balance creates an opportunity for migraines. Whichever you think is the better example? Would you choose one of those and get into specifics about the mechanics of it so folks can picture for themselves the role that endocannabinoid system plays in the ailment?
Ethan Russo: Sure. Let’s choose migraine. Now this is one of those situations where there’s a real danger of oversimplification because this is really complicated. For something that so many people get migraine is incredibly complex and to these days still poorly understood.
What we know is this. There’s no blood test for it. There’s nothing … No test specifically that tells you that someone has it but it’s totally based on the clinical pattern and that is the type of headache that’s often primarily one-sided. It tends to have a beating quality. It can be associated with nausea that can be very severe and it’s also associated with what are called photophobia and phonophobia. Respectively, those mean a sensitivity of the eyes to light and ears to sound.
Things that are normally not painful become painful to the patient having a migraine. Now this has a lot because it indicates that everything is geared up too high. It’s like the filters are off when somebody has this. They have this terrible pounding pain, nausea, sensitivity of eyes to light and ears to sound and it’s really a miserable condition.
What we know and this has been proven now. Given that I wrote my initial big paper on the clinical endocannabinoid deficiency in 2004, we have 11 years of subsequent research that actually shows that anandamide, one of the endogenous cannabinoids, is lower in people with migraine. This was done in the cerebrospinal fluid with spinal taps.
This is a study I had suggested way back when, but I didn’t think that it could be performed ethically in the United States. I guessed they were able to do it I’m Italy, because that’s exactly what they showed was that there was a significant lowering of anandamide in the spinal fluid of people with migraine as compared to those who didn’t have it. In essence that was the first I think real objective proof of clinical endocannabinoid deficiency.
It’s interesting because every symptom that I mentioned on relation to migraine seems to be alleviated pretty well by treatment with cannabis or to lesser extent THC on its own. When I was in neurology practice among my patients in practice and patients who reported to me about 80 percent of people who use cannabis to treat migraine seem to find it helpful both at the time taking it when they have a headache and especially as a preventive.
Now people may think that that’s new. It’s actually not. The first mention of this in the literature may have been 4,000 years ago if we read the science right from the ancient Acadian and Sumerian writings, but certainly we know this. Between by the 1840 and 1940, cannabis was a mainstream medicine both in Europe and the US. Actually, migraine was one of the most frequently reported uses for cannabis and great success was noted with those preparations. Now they had a lot of problems with quality control that won’t be evident now if medicine is made properly, so I think that this has great promise for the future.
Shango Los: For a patient who is self medicating and until the day comes that potentially there is an FDA-tested medicine out, what would you say would be the appropriate way for a patient to medicate? Do you think that an RSO preparation is appropriate? Do you think that actually smoking it so it takes effect more quickly? What is the method of delivery that you think is most likely to be effective?
Ethan Russo: It’s a complex topic. I mentioned earlier I think that the solution here is very low doses and so starting with the concentrate would be risky. What tends to happen there particularly for a medical patient especially in this context is it’s very easy to overshoot. A patient should be treating to the point of symptom control, not psycho-activity. Chances are with the concentrate the first inhalation is going to make them quite high and it might reduce their symptoms but maybe more than they need.
The ideal treatment to me in this situation is one that allows the patient to reduce their symptoms or eliminate them but still function. In other words people are not necessarily looking to have mental changes from their medicine. They’re looking for a relief and particularly for people who need to be working or studying it would be great to be able to get rid of the pain, nausea, et cetera and still be able to work, not feel high and certainly this can be done.
The approach would ideally be I think to have a medicine that was primarily cannabidiol perhaps a very small amount of THC and again use in a very sequential way, in other words very small amount to the point of benefit on symptoms and hopefully without psycho-activity.
Shango Los: What would you say the appropriate ratio would be something as simple as a 2 to 1 or as high of a CBD to THC ratio as you can manage?
Ethan Russo: Really the latter. Unfortunately, not all consumers who even have legal access in the states where they live are going to have reliable lab test on which to base their attempts of treatment. It really is what we call a therapeutic experiment. My best advice in all instances is to start low and go slow, particularly for the person who might have chronic frequent migraines.
Treating this preventively certainly should start with the lowest possible doses working up very slowly to the point that there’s benefit on the frequency and severity of the migraine attacks. Given that it’s a chronic condition ideally is to get better but get better slowly without creating side effects.
The problem with many cannabis-based medicines is particularly in naïve patients who hasn’t used cannabis before if their first experience is a bad one, which can happen particularly with concentrates, they may not return to it. They may have lost a good opportunity to successfully treat their condition. That would be a shame but that’s just one among many reasons that I think the slow what we call titration, slow increase in dose, is the best approach to this kind of clinical problem.
Shango Los: Now that we know that this kind of lack of balance has such an effect, what direction is the research going in? Now that we know that it exists, is the research moving towards how can we test for this without a spinal tap or is there some other area that’s hot right now?
Ethan Russo: That’s been slow and I’d like to help change that. I am hoping that n the next few years we can work with colleagues on doing brain imaging like I mentioned that would give us an idea of the state of someone’s endocannabinoid system. We can look with a special testing at levels in the blood of the endogenous cannabinoids and other conditions and see if we can produce correlations that would support that these are really important and how that disease works like I suspect is the case.
Because again this isn’t limited to migraine at all but certainly fibromyalgia, idiopathic bowel syndrome and possibly many others, including such common current problems as posttraumatic stress disorder. There’s very good evidence that there is an endocannabinoid deficiency operative in that disorder.
Shango Los: You said it earlier that the endocannabinoid system we’ve been aware of it for about 20 years and your cornerstone research on it that was published in 2004 and here we are now in 2015 and it’s just now finding its way out of academia and into citizen healer’s and patient’s knowledge. Why do you think that it’s taken so long for it to reach the patients?
Ethan Russo: It’s like anything else. Not everything gets noticed when it’s first mentioned. At the time I wrote the paper in 2004, there was not a lot of objective evidence. In the paper I try to assemble what was known about how these diseases worked and how they were affected by the endogenous cannabinoid system and by cannabis. Since then things have really changed and that as I mentioned there’s been the objective proof of an endocannabinoid deficiency in migraine. There’s been a lot of other evidence, too.
If I could talk about fibromyalgia for a minute this has a lot in common with migraine and they tend to happen in the same people. Fibromyalgia is a painful muscle spasm and pain condition. Now what it has in common with migraine is you can’t see anything. If you look at the tissues, it looks okay. If you scan it, it looks okay. Again, like migraine, there is pain on the proportion to what seems to be necessary. The pain can wander around the body. It can be quite disabling. It’s associated with a sleep disorder. Unfortunately, although it’s very common it’s treated very poorly by available medicines.
In 2014, the National Pain Report came out with a survey of 1,300 fibromyalgia patients and asking them how they responded to several agents. There are actually 3 drugs approved in the US to treat it. These are called duloxetine, milnacipran, and pregabalin. The first 2 are antidepressants that work on serotonin and norepinephrine, increasing the amounts of both. The third is an anticonvulsant, a seizure medicine that’s actually used to treat nerve-based pain.
However, these 1,300 patients who responded to the survey they found that these 3 drugs; duloxetine was very effective in only 8 percent, milnacipran in only 10 percent, and pregabalin in only 10 percent. They found that they got a little bit of help with duloxetine 32 percent, milnacipran 22 percent, and pregabalin 29 percent. However, people felt that they got no help at all from these drugs; duloxetine 60 percent, milnacipran 68 percent, and pregabalin 61 percent. This is pretty bad.
Now let’s compare with those people who used cannabis. 62 percent reported cannabis is very effective for this condition, so that’s 6 times better than any of the drugs that were approved for it. In the cannabis patients 33 percent additionally found that it helped a little and only 5 percent got no benefit at all.
Shango Los: Probably with a lot of side effects too.
Ethan Russo: Hopefully but one looks at the graph as I do in front of me it’s pretty readily apparent that there’s a big qualitative difference and that cannabis clearly is the best medicine as compared to the 3 FDA-approved drugs for this condition. Obviously, we need to do better and hopefully soon there will be legal access for cannabis-based medicine whether prescription or otherwise for other people that have condition, which is actually the most common diagnosis amongst dermatologists in the US, so it’s a very common condition.
Shango Los: Chances are we’re opening a lot of folks’ eyes to endocannabinoid deficiency just with our interview. For folks who are now interested in the topic and may want to find out more, it’s a pretty obscure topic. Where would you recommend that people go to find out more?
Ethan Russo: Hopefully, we can provide a URL to my study. There are lots of other studies. Additionally, we’ll be talking about this at Patients Out of Time conference coming up later in May in West Palm Beach, Florida. Eventually, a recording of the topic there which would be similar content to our discussion today will be online later that will also be available for continuing medical education credit so that patients could suggest that their doctors see this and they can get credit for it from watching it online. Additionally, because there’s been 11 years of additional research in this area I hope to write another article about this.
Shango Los: Fantastic. Dr. Russo, thank you for joining me today and thanks for sharing with us about endocannabinoid deficiency.
Ethan Russo: Thank you.
Shango Los: Dr. Ethan Russo is a world-renowned neurologist and cannabis researcher. I am Shango Los, founder of the Vashon Island Marijuana Entrepreneurs Alliance. Thank you for listening to Ganjapreneur.com.
Photo Credit: Natalie Martin
End